| Search Here : |
|
|
| Sponsor Links : |
|
|
| Make Donation To This Site: |
|
| My Directory: |



|
|
| Wednesday, January 24, 2007 |
| "THE TOP 10 QUALITIES OF A GOOD NURSE MANAGER" |

By Sandra A. Thompson, RN., BSN., (Case Manager at John C. Lincoln Hospital-North Mountain, in Phoenix, AZ).
References : AMERICAN JOURNAL NURSING, AGUST 2004, VOL. 104, NO. 8.
1.The number-one quality a good nurse manage must have : respect staff as professionals
Nothing is worse than being treated like a child in the work-place. A manager who disrespects her staff, especially in front of others, loses staff respect in return. Nurse managers should refrain from micromanagement; nurses are professionals who can think for themselves. Restraining or limiting nurses because of a lack of trust is deadly to the relationship between staff and manager. Nursing autonomy is promoted at the professional level; it must be promoted at the managerial level as well.
2.Set standards and a clear professional example.
Nurses are expected to behave professionally, and the same holds true for managers. A nurse manager needs to be professional in her appearance, language, and behavior, just as a staff nurse must be. Coming to work disheveled or inappropriately dressed, using improper language, or failing to follow standards for attendance or behavior are a few examples of the do-what-I-say-and-not-what-I-do double standard. What goes for the nurse must go for the manager.
3.Be organized, yet creative and flexible.
Many workers have unusual organizational methods, but employees are effected when a nurse manager can’t find an evaluation or forgets a deadline. The manager needs to be organized in a way that her staff can follow. She also needs to establish clear rules that she must be willing to adjust when necessary. For example, if a nurse’s child has a school event that conflicts with the posted schedule, the manager must understand its importance and try to resolve the dilemma. Of course, the manager must also recognize when staff members abuse such flexibility and set limits accordingly.
4.Be an effective decision maker, as well as a conflict and crisis manager.
The nursing staff expects the manager to make intelligent decisions when conflicts and problems arise. For example, managers should expect employees to attempt to resolve conflicts among them-selves. But manager needs to realize that she might be asked to assist. No one likes confrontations, but nurse managers who shrink from problems will only create more discord among the staff. When a serious problem arises on the unit, the nurse manager is looked to for leadership and support. If the manager responds by disappearing, crying, or exploding, the staff has diminished resources for handling problems. Timeliness is another factor. If the nurse manager judges too quickly or delays decisions, the entire unit suffers. Nursing staff and administrators agree that the ability to make good decisions is essential for a successful nurse manager.
5.Motivate and empower staff
Change is a necessary part of business, even the business of health care. The nurse manager needs to find ways to motivate and involve staff. If a nurse manager displays a hopeless, cynical, or dispassionate attitude, so will the staff nurses. The effective nurse manager is involved with the nursing staff on all levels, welcomes their input, and works with them to ensure excellence, create autonomy, and increase job satisfaction and opportunities for advancement.
6.Have a good sense of humor
Nursing is one of the toughest and most stressful jobs around. Tension can become so overwhelming that laughing is the only alternative to crying. An affective manager understands this; we are all human, and sometimes appropriate humor can be the healthiest and most compassionate way to help staff and patients cope.
7.Be honest, fair, consistent, and reasonable
Lying is one of the quickest ways to break someone’s trust, as is showing favoritism toward particular members of the staff. Deceit of any kind is devastating to the relationship between manager and staff. A good nurse manager knows that consistency matters-working for an unpredictable manager escalates tension and inhibits work. Being unreasonable in expectations and day-to-day dealings can also be harmful. A manager who wants to have an effective and cohesive team needs to be up front, realistic, and fair when it comes to interactions and expectations. Honest, sincere communication is always the best practice.
8.Be reliable resource and staff advocate
A nurse manager needs to have a solid clinical background, preferably in the specialty of the staff. Administrators often feel this is not necessary as long as the manager possesses strong managerial skills. From a staff nurse’s perspective, however, respect is lost if the manager is out of touch with what the specialized nursing staff does. The manager also needs to support nursing staff. A manager who does not back up staff loses their respect. A manager who supports staff and is an advocate for them gains loyalty.
9.Be available and accessible to staff
Admittedly, meetings and other managerial responsibilities are important, but the nursing staff needs to know that the manager is available when needed. Acknowledging and incorporating staff suggestions, whenever possible, is also important to nurses.
10.Be a great communicator
Effective communication is one of the most important tools for a leader or manager. Information should be conveyed in a clear manner. Staff should be informed of expectations and upcoming changes (not reprimanded after they’ve unknowingly done it wrong), be given timely and accurate information and updates, be listened to, and receive positive feedback, one of the most frequent complaints from nurses is that their managers only talk to them when they are in trouble. The nursing professions has a reputation for “eating its young,” and breaking this cycle can begin with positive interactions from the nurse manager.
While it’s the responsibility of the nurse manager to develop these qualities, staff nurses have a role in fulfillment of the top-10 list as well. What can staff nurses do to support these qualities in their nurse managers?
First, seek educational and practice opportunities to develop these attributes personally.
Second , communicate honestly with the nurse manager about your professional needs. Let the manager know what it is you need to be successful in providing good nursing care.
Third, patiently allow for mistakes and misjudgments, just as you would like manager to do for you. Above all, show respect, support, and appreciation especially when the manager has exhibited or practiced one of the qualities of a great nurse manager.
It’s logical that a good nurse manager will attract and retain nurses, and a bad one will drive them away. In light of the current nursing shortage, this issue becomes particularly important. What separates the good from the bad? Nurse managers who want to keep nurses will make it a priority to find out. Staff nurses who want good nurse managers will make it a priority to help them become so. |
Read More here ...
|
|
|
| Friday, December 29, 2006 |
| 7 Tips for a Better Night's Sleep |
Test your sleep IQ…
If you don’t sleep comfortably through the night, you’ll have a hard time waking up. Being groggy and cranky is not the ideal way to start out a brand new day full of possibilities. And even if you aim for eight full hours of sleep every night, you’re not guaranteed a restful night. So if you find that you wake up at odd hours of the night or constantly toss and turn during sleep, you could really use a better night’s sleep. Plus:
Dark, Quiet & Cool
The three fundamentals of a great night’s sleep are dark, quiet and cool.
To create a dark, quiet environment and get rid of distracting lights and sounds:
Shut all the curtains or blinds in your bedroom, and turn off the night light (you’re an adult now.)
If other family members are going to be staying up later than you and keeping the lights or television on, keep your door closed and ask them not to bother you once you’re in bed.
Open your window (as long as it’s quiet outside) or keep the fan or air conditioner on to keep a comfortably cool temperature in the room.
Achieving a dark, quiet and cool room will help your body realize it’s time for bed. It will also help you stay asleep longer.
Early Exercise
If you’re restless in the evening and can’t wind down by the time you climb into bed, it could be because you’re not using up enough energy during the day.
Believe it or not, exercising early on in the day helps you better utilize your energy stores during the day. It also boosts your metabolism and helps you think more clearly. Better yet, the old restless, agitated feeling you used to experience at night will be replaced by the need to rest your tired body and mind. By the end of a day that began with exercise, you'll be so exhausted that you won’t want to wait to hit the sack.
Food Police
Watch what you eat! Are you eating or drinking caffeinated foods late in the day? Do you eat too close to bedtime? Caffeine’s effects can last for up to seven hours, so lay off the caffeine after noon to ensure that any caffeine left in your system will be used up by the time you’re ready to lie down.
This includes coffee, chocolate and soda, which means that you may have to adjust your evening snack to something healthier, like fruit or popcorn, which is a win-win situation for your waistline.
Also, stop eating at least two hours before you go to bed. The digestive process can disrupt your sleep cycle and may even trigger strange dreams and nightmares.
Stress Less
Do the day’s events run through your head non-stop when all you want to do is shut off your mind and drift off to sleep? Letting stress get the better of you during the day can affect your sleep cycle, making a bad problem worse. Stress is also linked to countless diseases and a weakened immune system. For ideas on how to lower your stress levels, check out Learn How to Deal with Stress Effectively.
Get into a Routine
Think about how your heart beats – it’s a steady rhythm: bah-boom, bah-boom, bah-boom. Well your body craves routine too, particularly during the sleep cycle.
If you’re having a difficult time getting a full eight hours of sleep every night, set yourself some boundaries. If your bedtime is 10 p.m., and it takes you 30 minutes to fall asleep, set your alarm for 6:30 a.m. You’ll not only ensure that you will be getting a full eight hours of sleep every night, you’ll also give your body the routine it needs. And you’ll be able to tell when this routine becomes familiar to your body: You’ll be
sleepy by 10 p.m. every night.
you’re actually prolonging the time between crawling into bed and actually falling asleep. And if you’re not asleep, it doesn’t count as sleep time. TV also captivates the mind and the imagination, stimulating your brain with vibrant colors and sounds and keeping you awake longer. It can also affect the types of dreams you have.
If you really need some entertainment before bed, read a book under a soft light, which is sure to send you dozing in no time at all.
you’re actually prolonging the time between crawling into bed and actually falling asleep. And if you’re not asleep, it doesn’t count as sleep time. TV also captivates the mind and the imagination, stimulating your brain with vibrant colors and sounds and keeping you awake longer. It can also affect the types of dreams you have.
If you really need some entertainment before bed, read a book under a soft light, which is sure to send you dozing in no time at all.
Reference :
By Jennifer Gruenemay, ACE-Certified, LifeScript Staff Writer |
Read More here ...
|
|
|
|
| “Hypertension” |

Definition
Hypertension, commonly referred to as "high blood pressure", is a medical condition where the blood pressure is chronically elevated. While it is formally called arterial hypertension, the word "hypertension" without a qualifier usually refers to arterial hypertension. Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure and arterial aneurysm, and is a leading cause of chronic renal failure.
Hypertension can be classified as either essential or secondary. Essential hypertension is the term used when no specific medical cause can be found to explain a patient's condition. Secondary hypertension means that the high blood pressure is a result of (i.e. secondary to) another condition, such as kidney disease or certain tumours.
Recently, the JNC 7 (The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) has defined blood pressure 120/80 mmHg to 139/89 mmHg as "prehypertension." Prehypertension is not a disease category; rather, it is a designation chosen to identify individuals at high risk of developing hypertension.
The Mayo Clinic website indicates that your blood pressure is "normal if it's below 120/80" but that "some data indicate that 115/75 mm Hg should be the gold standard."
"In patients with diabetes mellitus or kidney disease studies have shown that blood pressure over 130/80 mmHg should be considered a risk factor and warrants treatment. Even lower numbers are considered diagnostic using home blood pressure monitoring devices. Contents
Hypertension means high blood pressure. This generally means:
Systolic blood pressure is consistently over 140 (systolic is the "top" number of your blood pressure measurement, which represents the pressure generated when the heart beats). Diastolic blood pressure is consistently over 90 (diastolic is the "bottom" number of your blood pressure measurement, which represents the pressure in the vessels when the heart is at rest). Either or both of these numbers may be too high.
Pre-hypertension is when your systolic blood pressure is between 120 and 139 or your diastolic blood pressure is between 80 and 89 on multiple readings. If you have pre-hypertension, you are likely to develop high blood pressure at some point. Therefore, your doctor will recommend lifestyle changes to bring your blood pressure down to normal range.
Etiology of Essential Hypertension
1. Environment
A number of environmental factors have been implicated in the development of hypertension, including salt intake, obesity, occupation, alcohol intake, family size, excessive noise exposure,[2] and crowding.
2. Salt Sensitivity
Sodium is the environmental factor that has received the greatest attention. It is to be noted that approximately 60% of the essential hypertension population is responsive to sodium intake.
3. Role of Rennin
Rennin is an enzyme secreted by the juxtaglomerular cells of the kidney and linked with aldosterone in a negative feedback loop.The range of plasma rennin activities observed in hypertensive subjects is broader than in normotensive individuals. In consequence, some hypertensive patients have been defined as having low-rennin and others as having high-rennin essential hypertension.
4. Insulin Resistance
Insulin is a polypeptide hormone secreted by the pancreas. Its main purpose is to regulate the levels of glucose in the body, it also has some other effects. Insulin resistance and/or hyperinsulinemia have been suggested as being responsible for the increased arterial pressure in some patients with hypertension. This feature is now widely recognized as part of syndrome X, or the metabolic syndrome.
5. Sleep Apnoea
Sleep apnoea is a common, under recognized cause of hypertension. It is best treated with weight loss and nocturnal nasal positive airway pressure.
6.Genetics
Hypertension is one of the most common complex genetic disorders, with genetic heritability averaging 30%. Data supporting this view emerge from animal studies as well as in population studies in humans. Most of these studies support the concept that the inheritance is probably multifactor or that a number of different genetic defects each have an elevated blood pressure as one of their phenotypic expressions.
More than 50 genes have been examined in association studies with hypertension, and the number is constantly growing.
7. Other Etiologies
There are some anecdotal or transient causes of high blood pressure. These are not to be confused with the disease called hypertension in which there is an intrinsic physiopathological mechanism as described above.
Etiology of Secondary Hypertension
Only in a small minority of patients with elevated arterial pressure can a specific cause be identified. These individuals will probably have an endocrine or renal defect that if corrected would bring blood pressure back to normal values.
1. Renal Hypertension
Hypertension produced by diseases of the kidney. A simple explanation for renal vascular hypertension is that decreased perfusion of renal tissue due to stenosis of a main or branch renal artery activates the renin-angiotensin system.
2. Adrenal Hypertension
Hypertension is a feature of a variety of adrenal cortical abnormalities. In primary aldosteronism there is a clear relationship between the aldosterone-induced sodium retention and the hypertension.
In patients with pheochromocytoma increased secretion of catecholamines such as epinephrine and norepinephrine by a tumor (most often located in the adrenal medulla) causes excessive stimulation of [adrenergic receptors], which results in peripheral vasoconstriction and cardiac stimulation. This diagnosis is confirmed by demonstrating increased urinary excretion of epinephrine and norepinephrine and/or their metabolites (vanillylmandelic acid).
3. Hypercalcemia
4. Coarctation of the Aorta
5. Diet
Certain medications, especially NSAIDS (Motrin/ibupofen) and steroids can cause hypertension. Ingestion of imported licorice (Glycyrrhiza glabra) can cause secondary hypoaldosteronism, which itself is a cause of hypertension.
Age. Over time, the number of collagen fibers in artery and arteriole walls increases, making blood vessels stiffer. With the reduced elasticity comes a smaller cross-sectional area in systole, and so a raised mean arterial blood pressure.
Pathophysiology
Most of the secondary mechanisms associated with hypertension are generally fully understood, and are outlined at secondary hypertension. However, those associated with essential (primary) hypertension are far less understood. What is known is that cardiac output is raised early in the disease course, with total peripheral resistance (TPR) normal; over time cardiac output drops to normal levels but TPR is increased. Three theories have been proposed to explain this:
Inability of the kidneys to excrete sodium, resulting in natriuretic factors such as Atrial Natriuretic Factor being secreted to promote salt excretion with the side-effect of raising total peripheral resistance.
An overactive renin / angiotension system leads to vasoconstriction and retention of sodium and water. The increase in blood volume leads to hypertension.
An overactive sympathetic nervous system, leading to increased stress responses.
Is is also known that hypertension is highly heritable and polygenic (caused by more than one gene) and a few candidate genes have been postulated in the etiology of this condition
Signs and symptoms
Hypertension is usually found incidentally - "case finding" - by healthcare professionals. It normally produces no symptoms. Malignant hypertension (or accelerated hypertension) is distinct as a late phase in the condition, and may present with headaches, blurred vision and end-organ damage. It is recognised that stressful situations can increase the blood pressure;
Hypertension is often confused with mental tension, stress and anxiety. While chronic anxiety is associated with poor outcomes in people with hypertension, it alone does not cause it.
Hypertensive urgencies and emergencies
Hypertension is rarely severe enough to cause symptoms. These typically only surface with a systolic blood pressure over 240 mmHg and/or a diastolic blood pressure over 120 mmHg. These pressures without signs of end-organ damage (such as renal failure) are termed "accelerated" hypertension. When end-organ damage is possible or already ongoing, but in absence of raised intracranial pressure, it is called hypertensive emergency. Hypertension under this circumstance needs to be controlled, but prolonged hospitalization is not necessarily required. When hypertension causes increased intracranial pressure, it is called malignant hypertension. Increased intracranial pressure causes papilledema, which is visible on ophthalmoscopic examination of the retina.
Complications
While elevated blood pressure alone is not an illness, it often requires treatment due to its short- and long-term effects on many organs. The risk is increased for:
Cerebrovascular accident (CVAs or strokes)
Myocardial infarction (heart attack)
Hypertensive cardiomyopathy (heart failure due to chronically high blood pressure)
Hypertensive retinopathy - damage to the retina
Hypertensive nephropathy - chronic renal failure due to chronically high blood pressure
Pregnancy
Main article: Hypertension of pregnancy
Although few women of childbearing age have high blood pressure, up to 10% develop hypertension of pregnancy. While generally benign, it may herald three complications of pregnancy: pre-eclampsia, HELLP syndrome and eclampsia. Follow-up and control with medication is therefore often necessary.
Diagnosis
1. Measuring blood pressure
Diagnosis of hypertension is generally on the basis of a persistently high blood pressure. Usually this requires three separate measurements at least one week apart. Exceptionally, if the elevation is extreme, or end-organ damage is present then the diagnosis may be applied and treatment commenced immediately.
Obtaining reliable blood pressure measurements relies on following several rules and understanding the many factors that influence blood pressure reading. For instance, measurements in control of hypertension should be at least 1 hour after caffeine, 30 minutes after smoking and without any stress. Cuff size is also important. The bladder should encircle and cover two-thirds of the length of the arm. The patient should be sitting for a minimum of five minutes. The patient should not be on any adrenergic stimulants, such as those found in many cold medications.
When taking manual measurements, the person taking the measurement should be careful to inflate the cuff suitably above anticipated systolic pressure. A stethoscope should be placed lightly over the brachial artery. The cuff should be at the level of the heart and the cuff should be deflated at a rate of 2 to 3 mmHg/s. Systolic pressure is the pressure reading at the onset of the sounds described by Korotkoff (Phase one). Diastolic pressure is then recorded as the pressure at which the sounds disappear (K5) or sometimes the K4 point, where the sound is abruptly muffled. Two measurements should be made at least 5 minutes apart, and, if there is a discrepancy of more than 5 mmHg, a third reading should be done. The readings should then be averaged. An initial measurement should include both arms. In elderly patients who particularly when treated may show orthostatic hypotension, measuring lying sitting and standing BP may be useful. The BP should at some time have been measured in each arm, and the higher pressure arm preferred for subsequent measurements.
BP varies with time of day, as may the effectiveness of treatment, and archetypes used to record the data should include the time taken. Analysis of this is rare at present. Automated machines are commonly used and reduce the variability in manually collected readings. Routine measurements done in medical offices of patients with known hypertension may incorrectly diagnose 20% of patients with uncontrolled hypertension .
Distinguishing primary vs. secondary hypertension
Once the diagnosis of hypertension has been made it is important to attempt to exclude or identify reversible (secondary) causes.
Over 90% of adult hypertension has no clear cause and is therefore called essential/primary hypertension. Often, it is part of the metabolic "syndrome X" in patients with insulin resistance: it occurs in combination with diabetes mellitus (type 2), combined hyperlipidemia and central obesity.
In hypertensive children most cases are secondary hypertension, and the cause should be pursued diligently.
Investigations commonly performed in newly diagnosed hypertension
Tests are undertaken to identify possible causes of secondary hypertension, and seek evidence for end-organ damage to the heart itself or the eyes (retina) and kidneys. Diabetes and raised cholesterol levels being additional risk factors for the development of cardiovascular disease are also tested for as they will also require management.
Blood tests commonly performed include:
Creatinine (renal function) - to identify both underlying renal disease as a cause of hypertension and conversely hypertension causing onset of kidney damage. Also a baseline for later monitoring the possible side-effects of certain antihypertensive drugs.
Electrolytes (sodium, potassium)
Glucose - to identify diabetes mellitus
Cholesterol
Additional tests often include:
Testing of urine samples for proteinuria - again to pick up underlying kidney disease or evidence of hypertensive renal damage.
Electrocardiogram (EKG/ECG) - for evidence of the heart being under strain from working against a high blood pressure. Also may show resulting thickening of the heart muscle (left ventricular hypertrophy) or of the occurrence of previous silent cardiac disease (either subtle electrical conduction disruption or even a myocardial infarction).
Chest X-ray - again for signs of cardiac enlargement or evidence of cardiac failure.
Epidemiology
The level of blood pressure regarded as deleterious has been revised down during years of epidemiological studies. A widely quoted and important series of such studies is the Framingham Heart Study carried out in an American town: Framingham, Massachusetts. The results from Framingham and of similar work in Busselton, Western Australia have been widely applied. To the extent that people are similar this seems reasonable, but there are known to be genetic variations in the most effective drugs for particular sub-populations. Recently (2004), the Framingham figures have been found to overestimate risks for the UK population considerably. The reasons are unclear. Nevertheless the Framingham work has been an important element of UK health policy.
Treatment
1. Lifestyle modification
Doctors recommend weight loss and regular exercise as the first steps in treating mild to moderate hypertension. These steps are highly effective in reducing blood pressure, although most patients with moderate or severe hypertension end up requiring indefinite drug therapy to bring their blood pressure down to a safe level. Discontinuing smoking does not directly reduce blood pressure, but is very important for people with hypertension because it reduces the risk of many dangerous outcomes of hypertension, such as stroke and heart attack.
Mild hypertension is usually treated by diet, exercise and improved physical fitness. A diet rich in fruits and vegetables and low fat or fat-free dairy foods and moderate or low in sodium lowers blood pressure in people with hypertension. This diet is known as the DASH diet (Dietary Approaches to Stop Hypertension), and is based on National Institutes of Health sponsored research. Dietary sodium (salt) may worsen hypertension in some people and reducing salt intake decreases blood pressure in a third of people. Regular mild exercise improves blood flow, and helps to lower blood pressure. In addition, fruits, vegetables, and nuts have the added benefit of increasing dietary Potassium, which offsets the effect of sodium and acts on the kidney to decrease blood pressure.
Reduction of environmental stressors such as high sound levels and over-illumination can be an additional method of ameliorating hypertension. Biofeedback is also used particularly device guided paced breathing
2. Medications
a. Antihypertensives
There are many classes of medications for treating hypertension, together called antihypertensives, which — by varying means — act by lowering blood pressure. Evidence suggests that reduction of the blood pressure by 5-6 mmHg can decrease the risk of stroke by 40%, of coronary heart disease by 15-20%, and reduces the likelihood of dementia, heart failure, and mortality from vascular disease.
The aim of treatment should be blood pressure control to <140/90 mmHg for most patients, and lower in certain contexts such as diabetes or kidney disease (some medical professionals recommend keeping levels below 120/80 mmHg)[4]. Each added drug may reduce the systolic blood pressure by 5-10 mmHg, so often multiple drugs are necessary to achieve blood pressure control.
Commonly used drugs include:
ACE inhibitors such as captopril, enalapril, fosinopril (Monopril®), lisinopril (Zestril®), quinapril, ramipril (Altace®)
Angiotensin II receptor antagonists: eg, irbesartan (Avapro®), losartan (Cozaar®), valsartan (Diovan®), candesartan (Atacand®)
Alpha blockers such as doxazosin, prazosin, or terazosin
Beta blockers such as atenolol, labetalol, metoprolol (Lopressor®, Toprol-XL®)
Calcium channel blockers such as amlodipine (Norvasc®), diltiazem, verapamil
Diuretics: eg, bendroflumethiazide, chlortalidone, hydrochlorothiazide (also called HCTZ)
Finally combination products (which usually contain HCTZ and one other drug)
Which type of many medications should be used initially for hypertension has been the subject of several large studies and various national guidlelines.
The ALLHAT study showed a slightly better outcome and cost-effectiveness for the thiazide diuretic chlortalidone compared to anti-hypertensives. Whilst a subsequent smaller study (ANBP2) did not show this small difference in outcome and actually showed a slightly better outcome for ACE-inhibitors in older male patients.[10]
Whilst thiazides are cheap, effective, and recommended as the best first-line drug for hypertension by many experts, they are not prescribed as often as some newer drugs. Arguably, this is because they are off-patent and thus rarely promoted by the drug industry.[11] Although physicians may start with non-thiazide antihypertensive medications if there is a compelling reason to do so. An example is the use of ACE-inhibitors in diabetic patients who have evidence of kidney disease, as they have been shown to both reduce blood pressure and slow the progression of diabetic nephropathy.[12] In patients with coronary artery disease or a history of a heart attack, beta blockers and ACE-inhibitors both lower blood pressure and protect heart muscle over a lifetime, leading to reduced mortality.
References :
Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164(19):2126-34.
Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Rockville, Md. National Heart, Lung, and Blood Institute, US Department of Health and Human Services; August 2004. National Institutes of Health Publication No. 04-5230.
Eyre H, Kahn R, Robertson RM, et al. Preventing cancer, cardiovascular disease, and diabetes: A common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. Circulation. 2004;109(25):3244-55.
Whelton PK, He J, Appel LJ, et al. Primary prevention of hypertension: Clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288(15):1882-8. |
Read More here ...
|
|
|
| Saturday, July 22, 2006 |
| "THE MESOTHELIOMA CANCER" |
Mesothelioma is a form of that is almost always caused by previous exposure to asbestos. In this disease, malignant (cancerous) cells develop in the mesothelium, a protective lining that covers most of the body's internal organs. Its most common site is the pleura (outer lining of the lungs and chest cavity), but it may also occur in the peritoium (the lining of the abdominal cavity) or thepericardium(a sac that surrounds the heart).
Most people who develop mesothelioma have worked on jobs where they inhaled asbestos particles, or have been exposed to asbestos dust and fibre in other ways, such as by washing the clothes of a family member who worked with asbestos, or by home renovation using asbestos cement products. There is no association between mesothelioma and smoking.
Signs and symptoms
Symptoms of mesothelioma may not appear until 20 to 50 years after exposure to asbestos. Shortness of breath, cough, and pain in the chest due to an accumulation of fluid in the pleural space are often symptoms of pleural mesothelioma.
Symptoms of peritoneal mesothelioma include weight loss and , abdominal swelling and pain due to ascites (a buildup of fluid in the abdominal cavity). Other symptoms of peritoneal mesothelioma may include bowel obstruction, blood clotting abnormalities, anemia, and fever. If the cancer has spread beyond the mesothelium to other parts of the body, symptoms may include pain, trouble swallowing, or swelling of the neck or face.
These symptoms may be caused by mesothelioma or by other, less serious conditions.
membrane surface to other parts of the body, such as the lymph nodes, lungs, chest wall, or abdominal organs.
Pathophysiology
The mesothelium consists of a single layer of flattened to cuboidal cells forming the epithelial lining of the serous cavities of the body including the peritoneal, pericardial and pleural cavities. Deposition of asbestos fibres in the parenchyma of the lung may result in the penetration of the visceral pleura from where the fibre can then be carried to the pleural surface, thus leading to the development of malignant mesothelial plaques. The processes leading to the development of peritoneal mesothelioma remain unresolved, although it has been proposed that asbestos fibres from the lung are transported to the abdomen and associated organs via the lymphatic system. Additionally, asbestos fibres may be deposited in the gut after ingestion of sputum contaminated with asbestos fibres.
Pleural contamination with asbestos or other mineral fibres has been shown to cause cancer. Long thin asbestos fibers (blue asbestos, amphibole,fibers) are more potent carcinogens than "feathery fibers" (chrysotile or white asbestos fibers. However, there is now evidence that smaller particles may be more dangerous than the larger fibers.They remain suspended in the air where they can be inhaled, and may penetrate more easily and deeper into the lungs. "We probably will find out a lot more about the health aspects of asbestos from [the World Trade Center attack], unfortunately," said Dr. Alan Fein, chief of pulmonary and critical-care medicine at North Shore-Long Island Jewish Health System. Dr. Fein has treated several patients for "World Trade Center syndrome" or respiratory ailments from brief exposures of only a day ortwo near the collapsed buildings.
Mesothelioma development in rats has been demonstrated following intra-pleural inoculation of phosphorylated chrysotile fibres. It has been suggested that in humans, transport of fibres to the pleura is critical to the pathogenesis of mesothelioma. This is supported by the observed recruitment of significant numbers of macrophages and other cells of the immune systemto localised lesions of accumulated asbestos fibres in the pleural and peritoneal cavities of rats. These lesions continued to attract and accumulate macrophages as the disease progressed, and cellular changes within the lesion culminated in a morphologically malignant tumour. Experimental evidence suggests that asbestos acts as a complete carcinogen with the development of mesothelioma occurring in sequential stages of initiation and promotion. The molecular mechanisms underlying the malignant transformation of normal mesothelial cells by asbestos fibres remain unclear despite the demonstration of its oncogenic capabilities. However, complete in vitro transformation of normal human mesothelial cells to malignant phenotype following exposure to asbestos fibres has not yet been achieved. In general, asbestos fibres are thought to act throughdirect physical interactions with the cells of the mesothelium in conjunction with indirect effects following interaction with inflammatory cells such as macrophages. Analysis of the interactions between asbestos fibres and DNA has shown that phagocytosed fibres are able to make contact with chromosomes, often adhering to the chromatin fibres or becoming entangled within the chromosome. This contact between the asbestos fibre and the chromosomes or structural proteins of the spindle apparatus can induce complex abnormalities. The most common abnormality is monosomy of chromosome 22. Other frequent abnormalities include structural rearrangement of 1p, 3p, 9p and 6q chromosome arms.
Asbestos fibres have been shown to alter the function and secretory properties of macrophages, ultimately creating conditions which favour the development of mesothelioma. Following asbestos phagocytosis, macrophages generate increased amounts of hydroxyl radicals, which are normal by-products of cellular anaerobic metabolism. However, these free radicals are also known clastogenic and membrane-active agents thought to promote asbestos carcinogenicity. These oxidants can participate in the oncogenic process by directly and indirectly interacting with DNA, modifying membrane-associated cellular events, including oncogene activation and perturbation of cellular antioxidant defences. Asbestos may also possess immunosuppressive properties. For example, chrysotile fibres have been shown to depress the in vitro proliferation of phytohemagglutinin-stimulated peripheral blood lymphocytes, suppress natural killer cell lysis and significantly reduce lymphokine-activated killer (LAK) cell viability and recovery. Furthermore, genetic alterations in asbestos-activated macrophages may result in the release of potent mesothelial cell mitogens such as platelet-derived growth factor (PDGF) and transforming growth factor-â (TGF-â) which in turn, may induce the chronic stimulation and proliferation of mesothelial cells after injury by asbestos fibres.
Epidemiology
Incidence
Although reported incidence rates have increased in the past 20 years, mesothelioma is still a relatively rare cancer. The incidence is approximately one per 1,000,000. For comparison, populations with high levels of smoking can have a lung cancer ncidence of over 1,000 per 1,000,000. Incidence of malignant mesothelioma currently ranges from about 7 to 40 per 1,000,000 in industrialized Western nations, depending on the amount of asbestos exposure of the populations during the past several decade. It has been estimated that incidence may have peaked at 15 per 1,000,000 in the United States in 2004. Incidence is expected to continue increasing in other parts of the world. Mesothelioma occurs more often in men than in women and risk increases with age, but this disease can appear in either men or women at any age. Approximately one fifth to one third of all mesotheliomas are peritoneal.
Between 1940 and 1979, approximately 27.5 million people were occupationally exposed to asbestos in the United States.Between 1973 and 1984, there has been a three-fold increase in the diagnosis of pleural mesothelioma in caucasion males. From 1980 to the late 1990s, the rate of deaths from mesothelioma increased from 2,000 to 3,000 a year. in the late 1990se in annual deaths from mesotheilioma. , with men four times more likely to acquire it than women. These rates may not be accurate, since it is possible that many cases of mesothelioma are misdiagnosed as adenocarcinoma of the lung, which is difficult to differentiate from mesothelioma.
Risk factors
Working with asbestos s the major risk factor for mesothelioma. A history of asbestos exposure exists in almost all cases. However, mesothelioma has been reported in some individuals without any known exposure to asbestos. In rare cases, mesothelioma has also been associated with irradiation, intrapleural thorium dioxide (Thorotrast), and inhalation of other fibrous silicates, such as erionite.
Asbestos is the name of a group of minerals that occur naturally as masses of strong, flexible fibers that can be separated into thin threads and woven. Asbestos has been widely used in many industrial products, including cement, brake linings, roof shingles, flooring products, textiles, and insulation. If tiny asbestos particles float in the air, especially during the manufacturing process, they may be inhaled or swallowed, and can cause serious health problems. In addition to mesothelioma, exposure to asbestos increases the risk of lung cancer, asbestosis (a noncancerous, chronic lung ailment), and other cancers, such as those of the larynx and kidney.
The combination of smoking and asbestos exposure significantly increases a person's risk of developing cancer of the airways (lung cancer,bronchial carcinoma). The Kent brand of cigarettes used asbestos in its filters for the first few years of production in the 1950s and some cases of mesothelioma have resulted. Smoking current cigarettes does not appear to increase the risk of mesothelioma.
Some studies suggest that simian virus 40 (SV40) may act as a in the development of mesotheliom.
Exposure
Asbestos has been mined and used commercially since the late . Its use greatly increased during World War II. Since the early 1940, millions of American workers have been exposedto asbestos dust. Initially, the risks associated with asbestos exposure were not publicly known. However, an increased risk of developing mesothelioma was later found among shipyard workers, people who work in asbestos mines and mills, producers of asbestos products, workers in the heating and construction industries, and other tradespeople. Today, the U.S. Occupational Safety and Health Administration(OSHA) sets limits for acceptable levels of asbestos exposure in the workplace, and created guidelines for engineering controls and respirators, protective clothing, exposure monitoring, hygiene facilities and practices, warning signs, labeling, recordkeeping, and medical exams. By contrast, the British Government's Health and Safety Executive (HSE) states formally that any threshold for mesothelioma must be at a very low level and it is widely agreed that if any such threshold does exists at all, then it cannot currently be quantified. For practical purposes, therefore, HSE does not assume that any such threshold exists. People who work with asbestos wear personal protective equipment to lower their risk of exposure.
Exposure to asbestos fibres has been recognised as an occupational health hazard since the early 1900. Several epidemiological studies have associated exposure to asbestos with the development of lesions such as asbestos bodies in the sputum, pleural plaques, diffuse pleural thickening, asbestosis, carcinoma of the lung and larynx, gastrointestinal tumours, and diffuse mesothelioma of the pleura and peritoneum.
The documented presence of asbestos fibres in water supplies and food products has fostered concerns about the possible impact of long-term and, as yet, unknown exposure of the general population to these fibres. Although many authorities consider brief or transient exposure to asbestos fibres as inconsequential and an unlikely risk factor, some epidemiologists claim that there is no risk threshold. Cases of mesothelioma have been found in people whose only exposure was breathing the air through ventilation systems. Other cases had very minimal (3 months or less) direct exposure.
Commercial asbestos mining at Wittenoom, Western Australia, occurred between 1945 and 1966. A cohort study of miners employed at the mine reported that while no deaths occurred within the first 10 years after crocidolite exposure, 85 deaths attributable to mesothelioma had occurred by 1985. It is predicted that the number of cases within this study group will reach in excess of 700 by the year 2020. By 1994, 539 reported deaths due to mesothelioma had been reported in Western Australia.
Family members and others living with asbestos workers have an increased risk of developing mesothelioma, and possibly other asbestos related diseases. This risk may be the result of exposure to asbestos dust brought home on the clothing and hair of asbestos workers. To reduce the chance of exposing family members to asbestos fibres, asbestos workers are usually required to shower and change their clothing before leaving the workplace.
Treatment
Treatment of MM using conventional therapies has not proved successful and patients have a median survival time of 6-12 months after presentation. The clinical behaviour of the malignancy is affected by several factors including the continuous mesothelial surface of the pleural cavity which favours local metastasis via exfoliated cells, invasion to underlying tissue and other organs within the pleural cavity, and the extremely long latency period between asbestos exposure and development of the disease.
Surgery
Surgery, either by itself or used in combination with pre- and post-operative adjuvant therapies has proved disappointing with a 5 year survival rate of less than 10%. A pleurectomy/decortication is the most common surgery, in which the lining of the chest is removed. Less common is an extrapleural pneumonectomy (EPP), in which the lung, lining of the inside of the chest, the hemi-diaphragm and the pericardium are removed.
Radiation
Although the tumor is highly resistant to radiotherapy, these regimens are sometimes used to relieve symptoms arising from tumor growth, such as obstruction of a major blood vessel.
Radiotherapy is commonly applied to the sites of chest drain insertion, in order to prevent growth of the tumor along the track in the chest wall.
Chemotherapy
In February 2004, the Food and Drug Administration approved pemetrexed (brand name Alimta) for treatment of malignant pleural mesothelioma.
Immunotherapy
Treatment regimens involving immunotherapy have yielded variable results. For example, intrapleural inoculation of Bacillus Calmette-Guérin (BCG) in an attempt to boost the immune response, was found to be of no benefit to the patient (while it may benefit patients with bladder cancer). Mesothelioma cells proved susceptible to in vitro lysis by LAK cells following activation by interleukin-2(IL-2), but patients undergoing this particular therapy experienced major side effects. Indeed, this trial was suspended in view of the unacceptably high levels of IL-2 toxicity and the severity of side effects such as fever and cachexia. Nonetheless, other trials involving interferon alpha have proved more encouraging with 20% of patients experiencing a greater than 50% reduction in tumor mass combined with minimalside effects.Heated Intraoperative Intraperitoneal Chemotherapy
A procedure known as heated intraoperative intraperitoneal chemotherapy was developed by Paul Sugarbaker at the Washington Cancer Institut. The surgeon removes as much of the tumor as possible followed by the direct administration of a chemotherapy agent, heated to between 40 and 48°C, in the abdomen. The fluid is perfused for 60 to 120 minutes and then drained.
This techniquepermits the administration of high concentrations of selected drugs into the abdominal and pelvic surfaces. Heating the chemotherapy treatment increases the penetration of the drugs into tissues. Also, heating itself damages the malignant cells more thanthe normal cells.
Legal issues
Asbestos litigation is the longest, most expensive mass tort in U.S. history, involving more than 6,000 defendants and 600,000 claimants. Current trends indicate that the rate at which people are diagnosed with the disease will likely increase though the next decade. Each year, 50,000 to 75,000 new asbestos-related lawsuits are filed. Analysts have estimated that the total costs of asbestos litigation in the USA alone will eventually reach $200 billion.See also asbestos and the law
History
The first lawsuit against asbestos manufacturers was brought in 1929. The parties settled that lawsuit, and as part of the agreement, the attorneys agreed not to pursue further cases. It was not until 1960 that an article published by Wagner et al in 1960 first officially established mesothelioma as a disease arising from exposure to crocidolite asbesto. The article referred to over 30 case studies of people who had suffered from mesothelioma in South Africa. Some exposures were transient and some were mine workers. In 1962 Dr McNulty reported the first diagnosed case of malignant mesothelioma in an Australian asbestos worke. The worker had worked in the mill at the asbestos mine in Wittenoom from 1948 to 1950.
In the town of Wittenoom, asbestos-containing mine waste was used to cover schoolyards and playgrounds. In 1965 an article in the British Journal of Industrial Medicine established that people who lived in the neighbourhoods of asbestos factories and mines, but did not work in them, had contracted mesothelioma.
Despite proof that the dust associatedwith asbestos mining and milling causes asbestos related disease, mining began at Wittenoom in 1943 and continued until 1966. It is difficult to understand why the mine and mill was allowed to initially open and operate without adequate risk control measures; and why nothing was done to force the owner (CSR) to clean them up, adopt safer work practices or close down their operations.
In 1974 the first public warnings of the dangers of blue asbestos were published in a cover story called "Is this Killer in Your Home?" in Australia's Bulletin magazine. In 1978 the Western Australian Government decided to phase out the town of Wittenoom, following the publication of a Health Dept. booklet, "The Health Hazard at Wittenoom", containing the results of air sampling and an appraisal of worldwide medical information.
By 1979 the first writs for negligence related to Wittenoom were issued against CSR and its subsidiary ABA, and the Asbestos Diseases Society was formed to represent the Wittenoom victims.
References:
- Http://www.wikipedia.org
- United States Department of Health and Human Services.
- "Cigarette smoking, asbestos exposure, and malignant mesothelioma" by Muscat JE, Wynder EL in Cancer Research (1991)
- "Soluble mesothelin-related protein--a blood test for mesothelioma" by B. W. Robinson, J. Creaney, R. Lake, A. Nowak, A. W. Musk, N. de Klerk, P.Winzell, K. E. Hellstrom and I. Hellstrom in Lung Cancer (2005)
- "Malignant mesothelioma and occupational exposure to asbestos: a clinicopathological correlation of 1445 cases" by V. L. Roggli, A. Sharma, K. J.Butnor, T. Sporn and R. T. Vollmer in Ultrastruct Pathol (2002)
. |
Read More here ...
|
|
|
| Friday, June 23, 2006 |
| “NURSING PROCEDURE : BLOOD TRANSFUSION” |
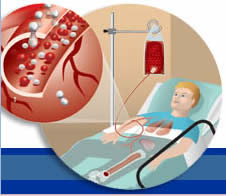
1.Definition
Is the introduction of whole blood or component of the blood, e.g. plasma or erythrocytes into venous circulation.
2.Blood Group
Human blood is classified in to four main groups (A, B, AB and O) on the basic of polysaccharide antigen on the erythrocyte surface. These antigens type A and Type B, commonly cause antibody reaction and are called agglutinogens. In other words group A blood contain type A agglutinogen, group B blood contain type B agglutinogen, group AB contain both A & B agglutinogens, and group O blood containe neither agglutinogen.
In addition to agglutinogens on the erythrocytes agglutinin (antibody) are present in the blood plasma. No individual can have agglutinin and agglutinogen of the same type, that person's system would attack its own cells. Then group A blood does not contain agglutinin A but does contain agglutinin B. Group B blood does not contain agglutinin B but does contain agglutinin A. Group AB blood contain neither agglutinin and group O contain both anti A and anti B agglutinin. Blood transfusion must be match to the patient blood type in term of compatible agglutinogen mismatch blood will cause hemolytic reaction.
Rhesus (Rh) and other factors
Rh antigen also on the surface of erythrocytes are present in about 85% of the population are can be a mayor cause of hemolytic reaction. Persons who possess the Rh factor are referred to as Rh positive those who do not are referred to as Rh negative.
Unlike the A and B agglitinogen, the Rh factor cannot cause a hemolytic reaction on the first exposure to mismatched blood, because the Rh antibody is not normally present in the plasma of Rh negative person.
3.Transfusion reaction
Transfusion reaction can be categorized as hemolytic, febrile, circulatory over load and allergic. The nurse must asses a client closely for reactions. Sign of an acute reaction include sudden chills or fever, low back pain, drop in blood pressure, nausea, flushing agitation or respiratory disorders. Sign of less severe allergic reaction include hives and itching but no fever.
Nursing management for transfusion reaction:
•Stop the transfusion. Maintain the intravenous line with normal saline solution
through new intravenous tubing, administered at a slow rate.
•Asses the patient carefully, compare the vital sign with those from the base line
assessment.
•Notify the physician of the assessment findings and implement any order obtained.
•Notify the blood bank that a suspected transfusion reaction has occurred.
•Send the blood container and tubing to the blood bank for repeat typing and
culture, the identifying tag and number are verified.
Before commencing a blood transfusion determine:
1.Base line data regarding blood pressure, temperature, pulse and respiration.
2.Any previous reaction to a blood transfusion.
3.The request for blood transfusion form has been completed and send specimen for
typing and cross matching, 3 ml in plain tube/red without wax or gel and 2 ml in
CBC tube.
4.Purpose
1.Restore blood volume after hemorrhage
2.Maintain hemoglobin levels in severe anemia
3.Replace specific blood component.
5. Assessment focus
Clinical signs of reaction (e.g. sudden chills, nausea, itching rash, dyspnea) status of infusion, site, any unusual symptoms.
Equipment
1.Unit of whole blood
2.Blood administration set either a straight line or a Y set ( Y set is preferred)
3.Normal saline solution
4.IV dressing
5.Vena puncture set containing a 18 needle or catheter, or if blood is to be
administered quickly no 16 needle or a larger.
6.Alcohol swab
7.Tape
8.Disposable gloves (Sterile)
6.Initiating, Maintaining and Terminating a Blood Transfusion
* Nursing Intervention
a.Pre Procedure
1.Obtain patient’s base line data before the transfusion.
•Asses base line data: Temp, Pulse, Respiration and Blood Pressure.
•Determine any known allergies or previous adverse reaction to blood.
Note specific signs related to the client's pathology and reason for transfusion
(e.g. an anemic client, note the hemoglobin level less than 10g/L).
2.Obtain the correct blood component for the patient.
•Check the physician's order with the requisition. See that doctor check and write
to start.
•Check the requisition form and the blood bag label with a specially check the
patient name, identification number, blood type and Rh group the blood donor
number, and the expiration date of blood.
•Ensure that doctor’s counter check and sign
•With another nurse (RN) compare the laboratory blood type round with :
•The client's name and identification number. Ask the patient to state the full name
as a double check.
•The number on the blood bag label
•The patient’s blood group and label, amount of blood, calculate and adjust.
•Check blood for any abnormalities, gas bubles dark color or cloudiness, clots and
excess air
•Make sure that the blood is left at room temperature for no more than 30 minutes
before starting the transfusion. RBCs deteriorate and lose their effectiveness
after 2 hours at room temperature. Agencies may designate different times at which
the blood must be returned to the blood bank if it has not been started. As blood
component warm, the risk of bacterial growth also increases.
Rational :
If the patient’s Clinical status permits, delay transfusion if baseline temperature is greater than 38.50 C
b.Procedure
1.Wash and dry hands
2.If any pre medication order, give before transfusion
3.Prepare the patient
•Identify the patient and explain the procedure and its purpose to the patient such
as blood product to be transfused, approximate length of time, and desired outcome
of transfusion.
4.Assemble the equipment and bring to the patient
5.Wear gloves.
6.Positioning the patient comfortably
7.Prime the tubing with saline solution.
Establish the saline infusion See that the set used in appropriate, as sometimes
attached filteris not suitable for some product
8.If the patient has an intravenous solution infusing check whether the needle and
solution are appropriate to administer blood. The needle should be no. 18 gauge or
larger and the solution must be saline. If solution is not compatible remove it
and dispose of it according to hospital policy. Dextrose which causes lysis of
RBCs, Ringer's Solution, medication and other additives and hyper alimentation
solution are incompatible.
9.If patient does not have an intravenous solution infusing, in the case you will
need to perform veni puncture on a suitable vein. Select a large vein that allows
patient some degree of mobility and place bed protector under the site. Start the
prescribed intravenous infusion
10.Establish the blood transfusion.
Invert the blood bag gently several times to mix the cell within the plasme
11.Start infusion slowly at 2 ml/mnt. Remain at bed side for 5-30 minutes. If there
are not sign of circulatory overloading, the infusion rate may be increased
12.Observe the patient closely for chilling, nausea, vomiting, skin rashes
tachycardia as they early sign and symptom reaction and check vital sign at
least hourly until 1 hour post transfusion. Report sign and symptoms of reaction
immediately to physician to minimize consequences. Acute reaction may occur at
anytime during the transfusion.If any reaction: close clamp & run normal saline,
report to doctor, save urine and observe.
Rational :
The majority of acute fatal transfusion reaction are caused by clerical errors. Patient and product verification is the single most important fucntion of the nurse. It is strongly recommended that two qualified individuals perform this task. Do not proceed with the transfusion if there is any discrepancy. Contact the blood bank immediately
cPost procedure
Obtain vital sign and compare with base line assessment.
Document procedure in patient's medical record including:
•Product , blood type Rh, volume transfused, rate, site infused.
•Product identification number
•Name of individual verifying, patient ID, name of person starting and ending
transfusion.
•Patient assessment findings and tolerance to procedure.
•Monitor patient for response to and effectiveness of the procedure.
Terminate the transfusion
Discard administration set according to policy procedure.
(i.e. If any reaction, save the set for further investigations)
Rational :
Rationale it must be possible to trace each transfusion product to the original blood donor. |
Read More here ...
|
|
|
| Tuesday, May 23, 2006 |
| "Liver Abcess Disease" |
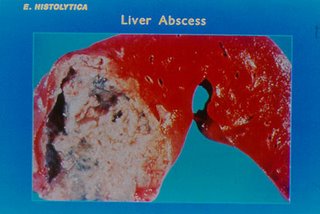
Basic Theory Liver Abcess
Two category : Amebic and pyogenic. Amebic liver abcess (commonly because Entamoeba histolytica), common cause on tropic or developing country.
Pathopysiology
Whenever an infection develops anywhere along the biliary of GI tract, infecting organism may reach the liver through the biliary system, portal venous system, or hepatic arterial or lymphatic system. The bacterial toxins destroy the neighboring liver cells, and resulting necrotic tissue serves as a protective wall for the organism.
Meanwhile, leucocytes migrate into infected area. Make abcess cavity full of a liquid, dead leucocytes and liver cell and bacteria. Pyogenic abcess of this type may be single, multiple and small. Examples of causes of pyogenic liver abcess include cholangitis and abdominal trauma.
Clinical manifestation
Fever with chills and diaphoresis, malaise, anorexia, nausea, vomiting, and weight loss may occur. Complaint dull abdominal pain and tenderness in the right upper quadrant abdomen. Hepatomegaly, jaundice, anemia, pleural effusion may develop. Sepsis and shock may be severe and life threatening.
Assessment and diagnostic finding
Blood culture are obtained but may not identify the organism. Aspiration of liver abcess guided US or CT scan, may be performed to assist in diagnosis and to obtain cultures of the organism. Percutaneous drainage of pyogenic abcess is carried out to evacuate abcess material and promote healing, with a catheter may be left in place for continues drainage.
Medical Management
Antibiotic iv therapy, the specific antibiotic use in treatment depends on the organism identified. Open surgical drainage may be required if antibiotic therapy and percutaneous drainage are ineffective.
NURSING CARE PLAN
Nursing Diagnoses :
1. Abdominal pain; discomfort R/T inserted liver drainage, process of diseases
2. Increased body temperature : hyperthermia, fever R/T infectious, presented abcess
3. Altered nutrition : less than body requirements R/T nausea, vomit, inadequate intake
4. Risk impaired skin integrity R/T inserted liver drainage tube
5. Potential Infectious large; septic R/T Inaddequate therapy, weakness
6. Anxiety R/T knowledge deficit about diseases and management therapy
Nursing objective :
1. Reduce pain : able torest, no complaint of pain and discomfort
2. Reduce fever : T normal
3 Provide adequate nutrition : adequate body weight, no vomit, Albumin normal
4. No inflammation on drainage area, sign of redness, adequate fixations
5. Healing of infectious, no signs septic, reduce : abcess drainage
6. No anxiety, ptn able to understands medication, management therapy and follow up treatment
Nursing Intervention
1. Abdominal pain; discomfort R/T inserted liver drainage, process of diseases
A. Asses and checked signs and complaint of pain
B. Suggested deeph breathing exercise and distraction technique
C. Apply compress on pain area
D. Suggest patients to take little food but frequent
E. Administered soft diet, low residu, and hepatic diet
C. Administered pain killer, analgesic as order
F. Administered antacid, zantac as order
2. Increased body temperature : hyperthermia, fever R/T infectious, presented abcess
A. Observed vital signs, monitor Temperature
B. Apply cold compress on axilla if fever
C. Administered antipiretic : panadol as order
D. Suggested increase oral intake
E. Administered IVF as order
F. Apply thick cloth or thick blanket
G. Sent all c/s screening as order
Altered nutrition : less than body requirements R/T nausea, vomit, inadequate intake, loss appetite
A. Asses frequent, appetite, type of diet or eating patient
B Assist ptn and encourage him to take food
C. Suggested ptn take diet frequently, little amount
D. Observed signs of vomit, nausea
F. Administered IVF as order
G. Measure body weight
H. Monitor lab : albumin, cholesterol
I. Administered anti emetic as order
4. Risk impaired skin integrity R/T inserted liver drainage tube
A. Observed patent of liver drainage
B. Observed signs redness, warm, or drainage condition on area of liver drainage
C. Do dressing with sterile technique daily with betadine and NS
D. Suggested ptn carefully during handling the liver tube, dont put bag more higher than abdomen area, do clamp as necessary
E. Daily changed clothe and linen
F. Suggested ptn not to removed or touch drain area
5. Potential Infectious large; septic R/T Inaddequate therapy, weakness
A. Observed and monitor output and condition of liver abcess drainage
B. Sent all diagnostic blood : CBC, ESR, blood c/s, liver abcess c/s, gram strain, differential etc
C. Administered antibiotic as order
D. Suggested ptn to follow up therapy
E. Informed diagnostic procedure ; U/S, blood report and drainage condition
F. Encourage high calorie high protein diet
6. Anxiety R/T knowledge deficit about diseases and management therapy
A. Assess patient knowledge about cause, prognosis, medication and treatment of diseases
B. Checked and assess signs of anxiety, un able to sleep
C. Explain about patient condition, cause, prognosis, management and supportive therapy
D. Suggested ptn to avoid alcohol drugs induced hepatotoksid
E. Explain that drainage will be d/c after less puss or drain and only temporary
F. To take all antibiotic as order
G. To prevent eat, drink from good source |
Read More here ...
|
|
|
| Saturday, April 29, 2006 |
| "Diabetes Mellitus" |

1. Definition
Diabetes is heteregeneous grup of disease involving the disruption of the metabolism of carbohidrates, fats, and protein.
2. Insuline Secretion and Function
Insuline is hormone secreted by the beta cells of the islet of Langerhans in the pancreas. Insulin is essential for celular metabolism of protein and fats.Through an internal feedback mechanism that involves the pancreas and the liver, circulating blood glucose level are maintained at normal range of 60 to 110 mg/dL.
3. Classification of Diabetes
a. Type 1 Diabetes Mellitus (Insulin Dependent Diabetes Mellitus-IDDM)
···Insulin needed to [revent ketosis, 5-10 % of all diabetic patient have type 1,
b. Type 2 : NIIDM (Non Insulin Dependent Diabetes Mellitus)
Formerly called "maturity -onset or adult onset diabetes.", maybe controlled with diet and oral hypoglycemics or insulin.
c. Type 3 : GDM (Gestational Diabetes Mellitus)
Glucose intolerance during pregnancy in women who were not known diabetics prior to pregnancy, will be reclassified after birth, may need to be
treated or may return to prepregnancy state and need no treatment.
d. Type 4 : Diabetes secondary to another condition, such as : pancreatic disease, other hormonal imbalanceor drug therapy such as involving glucocorticoids.
4. Pathophysiology
a. IDDM : absolute deficiency of insulin due to destruction of pancreatic beta cells by the interaction of genetic, immunologic, hereditary, or
enveronmental factors.
b. NIIDM : relative deficiency of insulin due to :
- An islet cells defect resulting in a slowed or delayed response in the release of insulin to a glucose load.
- or Reduction in the number of insulin receptors from continously elevated insulin level
- or A postreceptor defect
- or A major peripheral resistance to insulin induced by hypergliglycemia.
5. Risk Factor
a. Obisity
b. Family history of diabetes
c. Elderly
d. Women whose babies at birth weighed more than 9 lb.
e. History of autoimune disease.
6. Insulin Therapy
Insulin therapy involves the subcutaneous injection of short, intermediate or long actingat various times to achieve the desired effect. Short acting regular insulin can be given IV, There are about 20 insulins avalaible in the United States, mostly human insulin manufactured synthetically. Only about 6 % of diabetics are still using beef or pork insulin due to problem with immunogenicity.
# References :
1. The Lippincot manual of nursing practice-----7th Edition, edited by Sandra M. Nettina.
2. Little, Brown's NCLEX-RN, Examination Review,edited by Sally L.Lagerquist. |
Read More here ...
|
|
|
|
| Intravenous therapy |

Intravenous therapy or IV therapy is the administration of liquid substances directly into a vein. It can be intermittent or continuous; continuous administration is called an intravenous drip. The word intravenous simply means "within a vein", but is most commonly used to refer to IV therapy.
A. Indications :
1. Establish or maintain a fluid or electrolyte balance
2. Administer continuous or intermittent medication
3. Administer bolus medication
4. Administer fluid to keep vein open (KVO)
5. Administer blood or blood components
6. Administer intravenous anesthetics
7. Maintain or correct a patient's nutritional state
8. Administer diagnostic reagents
9. Monitor hemodynamic functions
B. IV Devices :
a. Steel Needles :
Example: Butterfly catheter. They are named after the wing-like plastic tabs at the base of the needle. They are used to deliver small quantities of medicines, to deliver fluids via the scalp veins in infants, and sometimes to draw blood samples (although not routinely, since the small diameter may damage blood cells). These are small gauge needles
b. Over the Needle Catheters
Example: peripheral IV catheter. This is the kind of catheter you will primarily be using. Also see the close up view of the catheter/needle tip in the next section ("inside the needle catheters").
Catheters (and needles) are sized by their diameter, which is called the gauge. The smaller the diameter, the larger the gauge. Therefore, a 22-gauge catheter is smaller than a 14-gauge catheter. Obviously, the greater the diameter, the more fluid can be delivered. To deliver large amounts of fluid, you should select a large vein and use a 14 or 16-gauge catheter. To administer medications, an 18 or 20-gauge catheter in a smaller vein will do.
C. IV Fluids :
Intravenous fluids are usually provided to:
- Provide volume replacement
- Administer medications, including electrolytes
- Monitor cardiac functions
For example, a patient comes into the ED with gastroenteritis and is dehydrated from vomiting and diarrhea. Acutely, she receives a fluid bolus to expand her intravascular volume. Her blood chemistry shows that her electrolytes are a bit off, so the IV fluid is adjusted to bring them within normal parameters. She is also given medication for nausea via her IV. She will remain on maintenance IV fluids until she is able to drink adequate amounts of fluids.
There are three main types of fluids:
- Isotonic fluids:
Can be helpful in hypotensive or hypovolemic patients.
Can be harmful. There is a risk of fluid overloading, especially in patients with CHF and hypertension.
Examples: Lactated Ringer's (LR), NS (normal saline, or 0.9% saline in water
- Hypotonic fluids:
Can be helpful when cells are dehydrated such as a dialysis patient on diuretic therapy. May also be used for hyperglycemic conditions like diabetic ketoacidosis, in which high serum glucose levels draw fluid out of the cells and into the vascular and interstitial compartments.
Can be dangerous to use because of the sudden fluid shift from the intravascular space to the cells. This can cause cardiovascular collapse and increased intracranial pressure (ICP) in some patients.
Example: .45% NaCl, 2.5% dextrose
- Hypertonic fluids :
Can help stabilize blood pressure, increase urine output, and reduce edema.
Rarely used in the prehospital setting. Care must be taken with their use. Dangerous in the setting of cell dehydration.
Examples: D5% .45% NaCl, D5% LR, D5% NS, blood products, and albumin.
Flow Rates :
You will often need to calculate IV flow rates. The administration sets come in two basic sizes:
1.Microdrip sets, Allow 60 drops (gtts) / mL through a small needle into the drip
chamber (Good for medication administration or pediatric fluid delivery).
2.Macrodrip sets, Allow 10 to 15 drops / mL into the drip chamber (Great for rapid
fluid delivery. Also used for routine fluid delivery).
3.Fluid may be ordered at a KVO rate. This means to Keep the Vein Open, or run in
fluids very slowly, enough to keep the vein open, but not really deliver much
volume.At times, you may desire a faster flow rate. This is usually expressed in
mLs / hour. In other words, how much fluid do you want your patient to receive
each hour? A common "maintenance" amount, for instance, would be "run it in at 125
an hour". Your patient would receive 125 mL of fluid every hour.
This is usually done by counting the number of drops that fall into the clear drip chamber on the IV administration set in one minute. To do this, you must know what size administration set you are using (micro or macrodrip). Plug the numbers into the following formula and you've got it!
(volume in mL) x (drip set) gtts
------------------------------------ = ------
(time in minutes) min
D. Vein Selection:
Veins of the Hand
1. Digital Dorsal veins
2. Dorsal Metacarpal veins
3. Dorsal venous network
4. Cephalic vein
5. Basilic vein
Veins of the Forearm
1. Cephalic vein
2. Median Cubital vein
3. Accessory Cephalic vein
4. Basilic vein
5. Cephalic vein
6. Median antebrachial vein
E. Technique:
Remember the four rights:Do I have the right patient?Do I have the right solution?Do I have the right drug?Do I have the right route?.
Preparation
It is important to gather all the necessary supplies before you begin. You will need: Absorbent disposable sheet, 1 alcohol prep pad, 1 betadine swab, Tourniquet, IV catheter, IV tubing, Bag of IV fluid. 4 pieces of tape (preferably paper tape or easy to remove tape which has been precut to approximately 4 inches (10cm) in length and taped conveniently to the table or stretcher. Disposable gloves, Gauze (several pieces of 4x4 or 2x2)
Prepare the IV fluid administration set.Inspect the fluid bag to be certain it contains the desired fluid, the fluid is clear, the bag is not leaking, and the bag is not expired.
Select either a mini or macro drip administration set and uncoil the tubing. Do not let the ends of the tubing become contaminated.Close the flow regulator (roll the wheel away from the end you will attach to the fluid bag).Remove the protective covering from the port of the fluid bag and the protective covering from the spike of the administration set.Insert the spike of the administration set into the port of the fluid bag with a quick twist. Do this carefully. Be especially careful to not puncture yourself!
Hold the fluid bag higher than the drip chamber of the administration set. Squeeze the drip chamber once or twice to start the flow. Fill the drip chamber to the marker line (approximately one-third full). If you overfill the chamber, lower the bag below the level of the drip chamber and squeeze some fluid back into the fluid bag. Open the flow regulator and allow the fluid to flush all the air from the tubing. Let it run into a trash can or even the (now empty) wrapper the fluid bag came in. You may need to loosen or remove the cap at the end of the tubing to get the fluid to flow although most sets now allow flow without removal. Take care not to let the tip of the administration set become contaminated.
Turn off the flow and place the sterile cap back on the end of the administration set (if you've had to remove it). Place this end nearby so you can reach it when you are ready to connect it to the IV catheter in the patient's vein.
Perform the venipuncture
Be sure you have introduced yourself to your patient and explained the procedure. Apply a tourniquet high on the upper arm. It should be tight enough to visibly indent the skin, but not cause the patient discomfort. Have the patient make a fist several times in order to maximize venous engorgement. Lower the arm to increase vein engorgement.
Select the appropriate vein. If you cannot easily see a suitable vein, you can sometimes feel them by palpating the arm using your fingers (not your thumb) The vein will feel like an elastic tube that "gives" under pressure. Tapping on the veins, by gently "slapping" them with the pads of two or three fingers may help dilate them. If you still cannot find any veins, then it might be helpful to cover the arm in a warm, moist compress to help with peripheral vasodilatation. If after a meticulous search no veins are found, then release the tourniquet from above the elbow and place it around the forearm and search in the distal forearm, wrist and hand. If still no suitable veins are found, then you will have to move to the other arm. Be careful to stay away from arteries, which are pulsatile.
Don disposable gloves. Clean the entry site carefully with the alcohol prep pad. Allow it to dry. Then use a betadine swab. Allow it to dry. Use both in a circular motion starting with the entry site and extending outward about 2 inches. (Using alcohol after betadine will negate the effect of the betadine) Note that some facilities may require an alcohol prep without betadine or sometimes alcohol after betadine. Go with the rules for your facility.
To puncture the vein, hold the catheter in your dominant hand. With the bevel up, enter the skin at about a 30 degree angle and in the direction of the vein. Use a quick, short, jabbing motion. After entering the skin, reduce the angle of the catheter until it is nearly parallel to the skin. If the vein appears to "roll" (move around freely under the skin), begin your venipuncture by apply counter tension against the skin just below the entry site using your nondominant hand. Many people use their thumb for this. Pull the skin distally toward the wrist in the opposite direction the needle will be advancing. Be carefully not to press too hard which will compress blood flow in the vein and cause the vein to collapse. Then pierce the skin and enter the vein as above.
Advance the catheter to enter the vein until blood is seen in the "flash chamber" of the catheter.
If not successful
If you are unsuccessful in entering the vein and there is no flashback, then slowly withdraw the catheter, without pulling all the way out, and carefully watch for the flashback to occur. If you are still not within the vein, then advance it again in a 2nd attempt to enter the vein. While withdrawing always stop before pulling all the way out to avoid repeating the painful initial skin puncture. If after several manipulations the vein is not entered, then release the tourniquet, place a gauze over the skin puncture site, withdraw the catheter and tape down the gauze. Try again in the other arm.
Otherwise,After entering the vein, advance the plastic catheter (which is over the needle) on into the vein while leaving the needle stationary. The hub of the catheter should be all the way to the skin puncture site. The plastic catheter should slide forward easily. Do not force it!!
(release the tourniquet)
Apply gentle pressure over the vein just proximal to the entry site to prevent blood flow. Remove the needle from within the plastic catheter. Dispose of the needle in an appropriate sharps container. NEVER reinsert the needle into the plastic catheter while it is in the patient's arm! Reinserting the needle can shear off the tip of the plastic catheter causing an embolus. Remove the protective cap from the end of the administration set and connect it to the plastic catheter. Adjust the flow rate as desired.
Tape the catheter in place using the strips of tape and a sterile 2X2 or a clear dressing. It is advisable not to use the "chevron" taping technique.
Label the IV site with the date, time, and your initials.Monitor the infusion for proper flow into the vein (in other words, watch for infiltration).
Occasionally, you may inadvertently enter an artery. You'll recognize this because bright red blood is quickly seen in the IV tubing and the IV bag because of the high pressure that exists. If this occurs, stop the fluid flow, remove the catheter, and put pressure on the site for at least 5 minutes.
To discontinue an IV
Remember to observe universal precautions. Start by clamping off the flow of fluids. Then gently peel the tape back toward the IV site. As you get closer to the site and the catheter, stabilize the catheter and remove the rest of the tape from the patient's skin. Then place a 4 x 4 gauze over the site and gently slide the plastic catheter out of the patient's arm. Use direct pressure for a few minutes to control any bleeding. Finally, place a band aide over the site.
Complications: Bruising, Cellulitis, Infiltrate, Extravasation, Phlebitis, Systemic Complications.
# Refences :
Steve Martin, PhD(c), PA-C
Nova Southeastern University PA Program |
Read More here ...
|
|
|
|
| Sponsor Links : |
|
| Nursing Links : |
|
| Doctor's Links : |
|
| Previous Post |
|
| Archives |
|
|
| Shoping Online : |
|
| Template by |

 |
|
